REPORT: Employer attitudes on GLP-1s, including coverage, costs, and outcomes
A recent report by Pharmaceutical Strategies Group (PSG), sponsored by Prescryptive, spotlighted red hot GLP-1s and how employers are thinking about these popular but expensive drugs. The annual Trends in Drug Benefit Design provides insights for employers about drug benefit design and management.
Findings: Employers are covering GLP-1 drugs while concerned about affordability
Important findings around the growth of GLP-1 drugs include:
- Over 90% of plans cover GLP-1 drugs for type 2 diabetes, while just over 30% cover these drugs for obesity.
- About three-quarters of plans have experienced increased GLP-1 drug spend in recent months.
- The most common strategies used to control costs related to coverage of GLP-1 drugs for obesity are prior authorization and a BMI requirement.
- The top reason for excluding GLP-1 drugs for obesity from coverage is belief that it would be too expensive to cover these drugs for all members for whom they would be prescribed.
- Only 1 in 10 plans that cover GLP-1 drugs for obesity are currently measuring outcomes
See the full report from PSG >

Obesity is a health crisis, and GLP-1s can help fight it
One reason that GLP-1s and other weight management strategies have been so popular is the rise in obesity – 43% of adults in the United States currently battle obesity, and this number is expected to rise to 50% by 2030. This has long-tail impacts in the American workforce. Due to associated comorbidities, obesity is calculated to be at least a $1.7 trillion disease, including $1.24 trillion in lost productivity and $480.7 billion in direct healthcare costs in the U.S. A person with obesity averages $1,861 in higher healthcare costs per year, compared to those with a healthy body weight.
Obesity is a health crisis, and it strains employees and employers.
A patient-centric approach can help create savings
As the PSG report found, 90% of plans surveyed cover GLP-1s for type 2 diabetes, but that number drop to just over 30% for obesity. The worry is that these drugs are expensive, which is understandable – and costs are going up.
A patient-centric approach to weight management can help create savings. In the legacy pharmacy benefit management system, organizations often prioritize rebates. Their formularies may favor a single highly rebated drug, leaving patients with limited options. But when a pharmacy benefits plan that focuses on lowering net cost can help the employer and the employee save and empower patients with choices that align with their circumstances.
See more reasons to take a patient-centric approach to weight management >
New technologies can help put the patient back in the prescription workflow
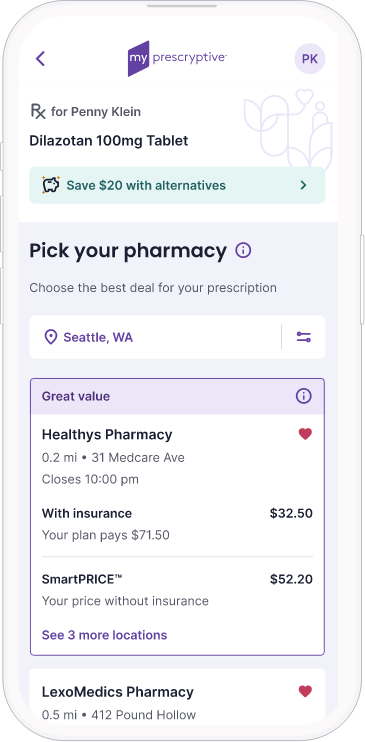
Isn’t it strange that out of all the things we shop for on our phones, from cars to houses, there’s no easy way to compare prescription drug prices? It’s all a mystery until the member gets to that pharmacy counter.
With digital prescription technology, patients can take control over their prescriptions from the doctor’s office and shop – cash vs insurance price, pharmacy location, less expensive alternatives – like they shop for everything else.
The PSG study found that only 1 in 10 plans that cover GLP-1 drugs for obesity are currently measuring outcomes. Let’s rewrite that script. The prescription is an opportunity to put members and patients on a sustainable, more affordable medication journey toward weight management – and control costs and adherence at the same time through data that gets shared back to the employer. It’s all possible with new technology.
Learn more about Prescryptive’s digital prescription >
More insights available in the full report
GLP-1s got a spotlight in this year’s report, but there’s so much more to discover! See more insights on drug benefit design, unbundling, drug pricing, utilization and more.
See the full PSG Trends in Drug Benefit Design report >