Not just another PBM.
This is emPBM.
When it comes to empowering your employees and members, a thoughtful approach matters. Increase engagement, enhance transparency, and drive up to 40% in plan savings.

9.7/10
employer satisfaction ratingwith Prescryptive transition
6x
less spent on prescription drugs by members who acted on Prescryptive real-time alerts
$2,564
average first-year total savings for plan per employee for prescription drug switches

Empowerment through technology
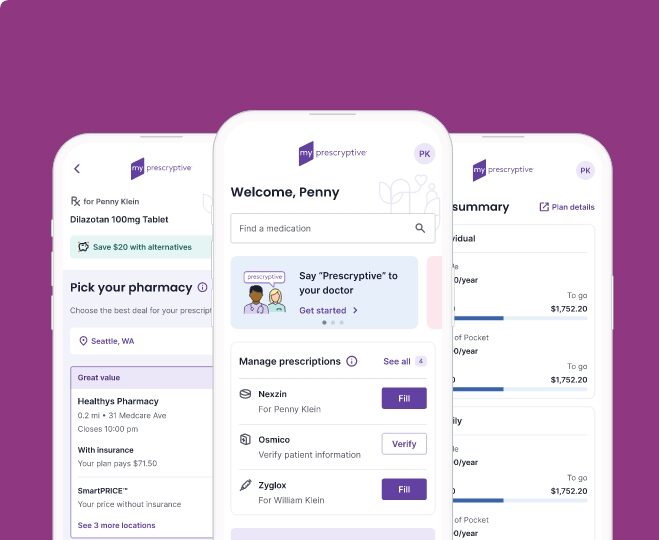
The Prescryptive Benefits Platform has member engagement built in
What makes emPBM by Prescryptive different than other PBMs? Gone are outdated strategies focused only on rebates that are not passed back to the plan or member. Our updated analysis and financial model reveals the true drug costs and opportunities members and employers have with emPBM.
The Prescryptive Formulary
Most PBMs would turn their nose up at the thought, but the benefits of a low net-cost strategy add up:
- Discourages higher-priced drugs to be included on a formulary
- Supports the use of lower cost drugs with the same or better efficacy
- Significantly enhances member’s ability to make the right choices for themselves, lower their cost, and the plan’s cost
Stop chasing rebates and choose emPBM: a new kind of PBM that saves self-funded employers and their employees money through a formulary strategy that’s transparent, effective and empowering.

Not replacing your PBM — revolutionizing it
“Before Prescryptive, we were fielding issues with our pharmacy benefit almost weekly.”
“[Costs are] 45% lower than when we started three years ago.”
News & Insights
Demystifying Prior Authorizations: Putting power back in healthcare consumers’ hands
In the complex world of healthcare, one of the most frustrating hurdles for healthcare consumers can be the…
Why digital prescription platforms like myPrescryptive are gaining national recognition
myPrescryptive, Prescryptive’s proprietary prescription management experience, showcases the best of what consumer-empowerment tools can offer healthcare consumers. What…
Prescryptive Named Gold Winner in the 2025 American Business Awards®
The company’s myPrescryptive mobile platform is now a multi-award winner with a Gold Stevie® for Best App –…
NCPDP 2025: Digital prescription solutions for better patient transparency
Miranda Rochol, Senior Vice President at Prescryptive Health, is leading the charge in transforming how healthcare consumers interact…
Connect with us
Want to bring transparency to your prescription process? Get in touch to see how.