Resources
If you’re a member, prescriber or pharmacy looking for forms, partner lists, policy documentation and more, keep scrolling for all the information you need, all in one place.
- Members
- Prescribers
- Pharmacy
Member resources
Our Member Services are available 24 hours a day, 365 days a year to answer questions about claims, initiate prior authorization for medications, and more.
Looking for your member account? Find it here.
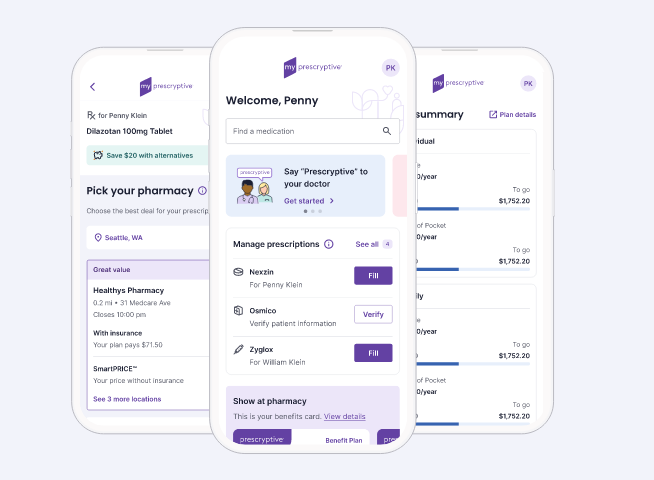
Set up your mobile account now
If you get pharmacy benefits through your employer, you can take full control of your prescriptions through our mobile-friendly member experience, myPrescryptive®.
Save on prescriptions with text alerts
Get real-time prescription alerts through myPrescryptive, with price information, pharmacy options, medication alternatives and other info that can save you money.
Set up mail order medications
Control and manage your retail pharmacy prescriptions from your phone with myPrescryptive. You also get to choose where and how you want to fill your prescriptions. For mail order prescriptions, view our list of mail order pharmacy partners.
Get started with specialty medications
We use a network of specialty medication pharmacies. First, learn about prior authorizations and understand the process with your healthcare provider, as specialty medications may require this process. Then work with our Customer Care team to get started: 1-206-686-9016.
Member Information
MARKETPLACE DRUG LIST – Four tier drug list guide to coverage.
Prescryptive members receive top-quality care and service from our pharmacy partners including thousands of retail pharmacies across the country. To find a network retail pharmacy in your neighborhood, login to your member portal and use your pharmacy finder tool.
Experience the convenience of home deliveries through one of our national mail order pharmacy partners. They are coordinated with your Prescryptive benefit for a hassle-free experience.
We use a network of specialty medication pharmacies. Specialty medications require a prior authorization before being covered. A prior authorization request form must be submitted by a healthcare provider on behalf of their patient to initiate the process.
With approval for a specialty medication, members receive complimentary access to specialty pharmacy care teams who work in partnership with your physician to ensure treatment adherence and success.
PRIOR AUTHORIZATION REQUEST FORM – Give this form to your healthcare provider to get a prior authorization review started.
MEMBER REIMBURSEMENT FORM – Use this form to be reimbursed for a claim you paid directly.
MEMBER APPEALS REQUEST FORM – Use this form to appeal a previous prior authorization decision.
APPEALS PROCESS – Learn how to use the appeals process.
EMERGENCY FILL POLICY – Learn our policy for addressing emergency prescription needs.
PRIVACY POLICY – Understand how your personal information is protected by Prescryptive.
Prescriber resources
Your patients will finally have access to true prescription pricing, at the point of care, so you can have more informed discussions about their options.
Retail pharmacy
For the first time, your patients can own their prescription with myPrescryptive. Patients can choose from 65,000+ pharmacies through our secure system and get their prescription as a text message directly on their phone to shop and select a pharmacy of their choice.
Mail order pharmacy
Prescryptive members who prefer the convenience of mail order can request home deliveries through one of our national mail order pharmacy partners.
Specialty pharmacy
Specialty medications require a prior authorization before being covered. A prior authorization request form must be submitted by a healthcare provider on behalf of their patient to initiate the process.
With approval for treatment with a specialty medication, patients have complimentary access to specialty pharmacy care teams who work in partnership with the patient’s physician to support treatment adherence and success.
Quick access resources
MARKETPLACE DRUG LIST – Four tier drug list guide to coverage.
PRIOR AUTHORIZATION REQUEST FORM – Give this form to your healthcare provider to get a prior authorization review started.
MEMBER APPEALS REQUEST FORM – Use this form to appeal a previous prior authorization decision.
APPEALS PROCESS – Learn how to use the appeals process.
EMERGENCY FILL POLICY – Learn our policy for addressing emergency prescription needs.
MARKETPLACE PRIOR AUTHORIZATION CRITERIA – Understand prior authorization review policies.
Pharmacy resources
It’s not just our technology that makes it easier for you to get your job done. Find the forms, codes, policy documentation and more that you’ll need below.
Contact Support
For pharmacy network or billing questions:
pharmacyrelations@prescryptive.com
Fraud Hotline: 1-206-800-2133
Pharmacy benefit resources
MARKETPLACE DRUG LIST – Four tier drug list guide to coverage.
EMERGENCY FILL POLICY – Learn our policy for addressing emergency prescription needs.
MARKETPLACE PRIOR AUTHORIZATION CRITERIA – Understand prior authorization review policies.
EFT/ACH FORM – Fill out to receive payments for all claims electronically via ACH.
PHARMACY ENROLLMENT FORM – Fill out to join our national network.
PHARMACY APPEALS AND GRIEVANCES FORM – Fill out to provide documentation for appeals and grievances.
TENNESSEE PHARMACY REIMBURSEMENT APPEAL FORM – Complete form for all prescription drugs or devices in Tennessee for which payment received is less than actual cost.
PRESCRYPTIVE PHARMACY PROVIDER MANUAL – Provides regulatory, administrative, and billing guidance to pharmacies in the Prescryptive network.
PRESCRYPTIVE PRICING PAYER SHEET – NCPDP requirements for submission of cash claims for adjudication.
PRESCRYPTIVE HEALTH COMMERCIAL PAYER SHEET – NCPDP requirements for submission of commercial claims.